- Spine Care
- Carpal Tunnel Syndrome / Cubital Tunnel Syndrome
- Concussion and Traumatic Brain Injury
- Stroke Rehab
- Tendonitis
- Spasticity Management
- Joint Pain
- Amputation and limb deficiencies
- Spinal Cord Rehab
- Hospital
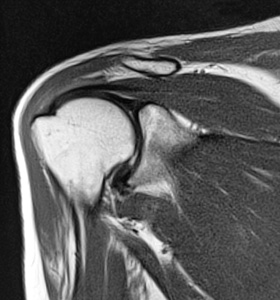
SPINE CARE: NECK AND BACK PAIN, PINCHED NERVES/RADICULOPATHY, DISC PROBLEMS, ARTHRITIS OF THE SPINE, MUSCULAR STRAIN
 We could write a novel on this topic. Spine Care has many avenues of treatment. Our philosophy as rehab physicians is simple. First it is important to CORRECTLY DIAGNOSE and EDUCATE the patient as to what the source of pain is in their neck, back, and/or extremities. This involves a thorough and focused history, exam, and may require appropriate testing including MRI’s, XRAYs, and/or EMG/NCS studies also known as nerve tests. Once you have your diagnosis our plan is to resolve your pain in the LEAST INVASIVE WAY possible. This often includes medications management as well as therapy. Our goal is to return you to your pain free days and attempt to make you even MORE ACTIVE than you were before all while avoiding needles and surgeries if possible. Surgery is necessary for certain conditions and can be helpful in preventing irreversible damage. We do not hesitate to refer patients on to surgery when it is needed. However our goal is to see if there are any measures we can take PRIOR to that in order to prevent invasive action. Many patients have never heard of Rehab Doctors or Physical Medicine and Rehabilitation Physicians until they visit our doctors. As Rehab Doctors our goal is to try rehab the patient back to their normal activity level if not a higher one.
We could write a novel on this topic. Spine Care has many avenues of treatment. Our philosophy as rehab physicians is simple. First it is important to CORRECTLY DIAGNOSE and EDUCATE the patient as to what the source of pain is in their neck, back, and/or extremities. This involves a thorough and focused history, exam, and may require appropriate testing including MRI’s, XRAYs, and/or EMG/NCS studies also known as nerve tests. Once you have your diagnosis our plan is to resolve your pain in the LEAST INVASIVE WAY possible. This often includes medications management as well as therapy. Our goal is to return you to your pain free days and attempt to make you even MORE ACTIVE than you were before all while avoiding needles and surgeries if possible. Surgery is necessary for certain conditions and can be helpful in preventing irreversible damage. We do not hesitate to refer patients on to surgery when it is needed. However our goal is to see if there are any measures we can take PRIOR to that in order to prevent invasive action. Many patients have never heard of Rehab Doctors or Physical Medicine and Rehabilitation Physicians until they visit our doctors. As Rehab Doctors our goal is to try rehab the patient back to their normal activity level if not a higher one.
CARPAL TUNNEL SYNDROME, CUBITAL TUNNEL SYNDROME, HAND PAIN and NUMBNESS
 Carpal Tunnel Syndrome is a common cause of Numbness, Tingling, Pain, and/or Weakness in the hand. Typically it involves numbness and/or tingling of the thumb, index, middle, and part of the ring finger HOWEVER it can involve the entire hand and cause pain all the way up to the shoulder. The cause is a nerve (median nerve) being entrapped at the wrist. It is often diagnosed by a combination of history, physical exam, and sometimes nerve conduction studies (aka EMG/NCS). Cubital Tunnel Syndrome is a result of the ulnar nerve being entrapped at the elbow. Typically this will cause numbness/tingling of the 4th and 5th digit as well as weakness of the hand. This also is often diagnosed by history, physical exam, and nerve conduction studies (aka EMG/NCS). There are other causes however for numbness, tingling, pain, and/or weakness of the hand. The vast differential diagnosis includes a pinched nerve in the neck, referred pain from a muscular dysfunction, and thoracic outlet syndrome (albeit it rare) to name a few. In order to fix your problem it is imperative that you first correctly diagnose your issue. Our physicians are experts in the neuromuscular system and its treatment which often includes therapy.
Carpal Tunnel Syndrome is a common cause of Numbness, Tingling, Pain, and/or Weakness in the hand. Typically it involves numbness and/or tingling of the thumb, index, middle, and part of the ring finger HOWEVER it can involve the entire hand and cause pain all the way up to the shoulder. The cause is a nerve (median nerve) being entrapped at the wrist. It is often diagnosed by a combination of history, physical exam, and sometimes nerve conduction studies (aka EMG/NCS). Cubital Tunnel Syndrome is a result of the ulnar nerve being entrapped at the elbow. Typically this will cause numbness/tingling of the 4th and 5th digit as well as weakness of the hand. This also is often diagnosed by history, physical exam, and nerve conduction studies (aka EMG/NCS). There are other causes however for numbness, tingling, pain, and/or weakness of the hand. The vast differential diagnosis includes a pinched nerve in the neck, referred pain from a muscular dysfunction, and thoracic outlet syndrome (albeit it rare) to name a few. In order to fix your problem it is imperative that you first correctly diagnose your issue. Our physicians are experts in the neuromuscular system and its treatment which often includes therapy.
Tendonitis: Shoulder, Knee, Hand, Foot/Achilles Pain
 Tendonitis is inflammation and swelling of the tendons that connect muscles to bones. Tendons often become injured during strenuous physical activities or after non-strenuous repetitive movements are performed. This usually results in pain near joints where the tendons attach to bones. Swelling of the soft tissues near the injured tendons as well as some weakness in nearby muscles may also occur. Tendonitis is commonly diagnosed after a physical examination but sometimes imaging of the tendon and joint are needed. There are many treatments for tendonitis that include oral or topical medications, injections near the affected tendon, stretching and strengthening exercises, bracing, and activity modifications.
Tendonitis is inflammation and swelling of the tendons that connect muscles to bones. Tendons often become injured during strenuous physical activities or after non-strenuous repetitive movements are performed. This usually results in pain near joints where the tendons attach to bones. Swelling of the soft tissues near the injured tendons as well as some weakness in nearby muscles may also occur. Tendonitis is commonly diagnosed after a physical examination but sometimes imaging of the tendon and joint are needed. There are many treatments for tendonitis that include oral or topical medications, injections near the affected tendon, stretching and strengthening exercises, bracing, and activity modifications.
Joint Pain: Shoulder, Hand, Elbow, Knee, Hip, Foot
 Joint pain is a common aliment that affects the physical function and quality of life of many individuals. There are many causes of joint pain including traumatic injury or systemic disease; however, most cases of joint pain are caused by inflammation and/or degeneration of bones and other supporting soft tissues such as cartilage or ligaments. Pain can occur in any joint in the body but the hands, shoulders, knees, and hips are commonly affected. Some types of joint pain are referred to as “arthritis.” Osteoarthritis is the most common form of arthritis and can cause pain inside the joints. It often occurs as a person ages and usually results from the breakdown of cartilage, which is the padding between bones. It is important to understand the cause of joint pain so that it can be treated appropriately. This is usually done by physical examination, imaging of the joint, and occasionally blood tests. Sometimes joint pain requires surgery; however, there many non-surgical treatment options for joint pain. These include oral or topical medications, joint injections, bracing, lifestyle modifications, and exercises to strengthen the muscles supporting the joint.
Joint pain is a common aliment that affects the physical function and quality of life of many individuals. There are many causes of joint pain including traumatic injury or systemic disease; however, most cases of joint pain are caused by inflammation and/or degeneration of bones and other supporting soft tissues such as cartilage or ligaments. Pain can occur in any joint in the body but the hands, shoulders, knees, and hips are commonly affected. Some types of joint pain are referred to as “arthritis.” Osteoarthritis is the most common form of arthritis and can cause pain inside the joints. It often occurs as a person ages and usually results from the breakdown of cartilage, which is the padding between bones. It is important to understand the cause of joint pain so that it can be treated appropriately. This is usually done by physical examination, imaging of the joint, and occasionally blood tests. Sometimes joint pain requires surgery; however, there many non-surgical treatment options for joint pain. These include oral or topical medications, joint injections, bracing, lifestyle modifications, and exercises to strengthen the muscles supporting the joint.
Spinal Cord Rehab
 The spinal cord is a bundle of nerves that starts at the base of the head and extends all the way down your back. These nerves are responsible for sensation to the body and carry signals from the brain to the muscles that coordinate movements. The spinal cord is protected by bones called vertebrae. Collectively, the bones and bundle of nerves make up the spine.
The spinal cord is a bundle of nerves that starts at the base of the head and extends all the way down your back. These nerves are responsible for sensation to the body and carry signals from the brain to the muscles that coordinate movements. The spinal cord is protected by bones called vertebrae. Collectively, the bones and bundle of nerves make up the spine.
The spine is divided into 4 regions: cervical, thoracic, lumbar, and sacral. The cervical region can be thought of as the bones and nerves of the neck. The cervical nerves are involved in controlling breath-ing, sensation and movements of the arms. The thoracic region is from the base of the neck to the level of the last rib. The thoracic nerves connect to muscles that assist in coughing, breathing, and trunk stabilization. The lumbar region is commonly referred to as the low back area. These nerves control sensation and movements of the legs and feet. Lastly, the sacral region is where the nerves of the tail bone live. The sacral nerves are also partly responsible for some sensation to the legs and feet. More importantly, these nerves stimulate the colon, rectum, bladder, and genital organs.
Injury to the spinal cord can occur from either traumatic or non-traumatic causes. Trauma to the spinal cord can be from motor vehicle crashes, falls, sports, and violence. Non-traumatic injuries of the spinal cord can be due to narrowing of the spinal canal from spinal stenosis, disc herniation, and degenerative changes of the of the spine. It is important to recognize that a spinal cord injury itself can occur with or without damage to the surrounding bones.
Spinal cord injuries can be further classified as complete or incomplete injuries. Complete injuries mean that there are no longer connections to the muscles that are located after the site of injury. Whereas, incomplete injuries still have some working connections to the muscles that are stimulated farther down the spinal cord after the injury. These classifications give doctors a better idea as to the likelihood of motor recovery.
Regardless of the type or completeness of injury, rehabilitation is the key to helping people with spinal cord injuries learn techniques and skills that help them get back to the activities they enjoy doing. There will be multi-disciplinary team to support individuals during their journey. The team will include physical therapists, occupational therapists, social workers, nurses and your doctor. The rehabilitation team which is led by one of our physicians will work hard with you and your family for safe return home and integration back into the community. Once home the rehab endeavors will continue and be managed by one of our physicians.
Stroke Rehab
 A stroke occurs when there is a lack of blood flow and subsequently oxygen to the brain. Risk factors for stroke include: older age, male, family history of stroke, hypertension, diabetes mellitus, heart disease, carotid stenosis, tobacco use, and alcohol and cocaine abuse.
A stroke occurs when there is a lack of blood flow and subsequently oxygen to the brain. Risk factors for stroke include: older age, male, family history of stroke, hypertension, diabetes mellitus, heart disease, carotid stenosis, tobacco use, and alcohol and cocaine abuse.
There are two main types of strokes: ischemic and hemorrhagic. Ischemic strokes happen due to a blockage of a major or minor artery in the brain, or from a blood clot formed in a distant part of the body that migrates to the brain. Hemorrhagic strokes happen secondary to weakened blood vessels that can leak or burst leading to blood accumulation that can compress and damage surrounding brain tissue.
Both types of strokes can result in many complications such as: weakness on one side of the body, difficulty speaking, difficulty swallowing, difficulty thinking, bowel and bladder dysfunction, pain, blood clots, and/or depression.
Stroke rehabilitation is focused on enhancing community integration and functional independence with everyday tasks such as getting dressed, showering, going to the bathroom, and walking. During rehabilitation one of our rehab physicians will try to prevent, address, and treat the secondary complications listed above if present. However, it is important to mention that the care of post-stroke survivors is through a multi-disciplinary team. This team includes speech therapists, occupation therapists, physical therapists, social workers, nurses, and doctors. Collaboratively, the team will also work to understand each patient’s equipment and home needs to ensure a safe transition to home if possible. Recovery can continue even up to a year after the rehabilitation course is completed. Thus, there will a continued relationship with your rehabilitation physician on an outpatient basis if needed.
Concussion and Traumatic Brain Injury
 Concussion is a term typically used when referring to a head injury sustained during sport activities but is widely used to describe trauma to the head sustained in a fall or being struck by an object. Often imaging is negative. Concussions are considered a mild traumatic brain injury (TBI). The American Con-gress of Rehabilitation (1995) defined mild TBI as “a traumatically induced physiological disruption of brain function which can manifest as loss of consciousness, and loss of memory for events immediately before or after the injury, and alteration in mental status at the time of accident, focal or neurological deficits which may or may not be transient.”
Concussion is a term typically used when referring to a head injury sustained during sport activities but is widely used to describe trauma to the head sustained in a fall or being struck by an object. Often imaging is negative. Concussions are considered a mild traumatic brain injury (TBI). The American Con-gress of Rehabilitation (1995) defined mild TBI as “a traumatically induced physiological disruption of brain function which can manifest as loss of consciousness, and loss of memory for events immediately before or after the injury, and alteration in mental status at the time of accident, focal or neurological deficits which may or may not be transient.”
Typical symptoms following a mild TBI include: headache, dizziness, ringing in the ear, hearing loss, blurred vision, altered taste or smell, sleep disturbance, insomnia, fatigue, sensory impairments, attention and concentration deficits, slow mental processing, memory impairments, lability, irritability, depression, and/or anxiety. Generally most patients recover within 3 months following injury. Persistent symptoms greater than 3 months are said to have Postconcussion Syndrome.
There are 3 major guideline used for grading concussion and return to play: Cantu, Colorado Medical Society and American Academy of Neurology.
More severe traumatic head injuries can result in severe cognitive deficits and at times include coma. Generally duration of coma predicts outcomes of patients with 2 weeks as the threshold mark for prognostication of recovery.
Traumatic brain injury can present as subdural hematoma, epidural hematoma, intraventricular hemorrhage or diffuse axonal injury. Impairments will vary based on the injury but can include weakness, paralysis, spasticity, difficulty swallowing or communicating, agitation, memory impairment and/or behavioral issues.
Following injury, patients may need inpatient rehab, long term acute care hospitalizations, or skilled nursing facility before discharging to home. Often, outpatient therapy will need to be continued to work toward improving function. Recovery from a TBI may take months to years with many often struggling with significant disability due to cognitive and memory problems and physical impairments. Caregiver burden is high due to the level of supervision and amount of physical assistance that may be needed. Our physicians are highly trained in managing all forms of TBIs and will work closely with therapy and nursing staff both on the inpatient and outpatient side to assist the patient in recovery.
Spasticity Management
 Spasticity is velocity dependent increase in muscle tone in response to stretch. This is commonly and mistakenly identified as “muscle spasm”. Generally, spasticity develops secondary to neurological events such as strokes, traumatic brain injury, multiple sclerosis, and/or spinal cord injury. Muscle spasms are typical used to describe pain in the muscle due to injuries to the back and limb.
Spasticity is velocity dependent increase in muscle tone in response to stretch. This is commonly and mistakenly identified as “muscle spasm”. Generally, spasticity develops secondary to neurological events such as strokes, traumatic brain injury, multiple sclerosis, and/or spinal cord injury. Muscle spasms are typical used to describe pain in the muscle due to injuries to the back and limb.
Spasticity is often presents in several ways. Typically, patient may note difficult in performing certain actions, limbs may be fixed in a certain position, movement may be associated with writhing or twisting movement (dystonia) or involuntary repeated movements of the hand or feet may be noted (clonus).
A good example of spasticity that can be seen is in a patient who presents with a history of stroke. Initially following a stroke, patient’s limb can be very loose (flaccid) and progressively over time more tone is noted and the arm begins to draw up bent at the elbow. In normal muscle contraction, when we want to flex the elbow this is done in a smooth, controlled fashion. In the case of stroke, the coordination of two muscles is not normal which leads us to two common scenarios. One scenario is one muscle may overpower another muscle resulting in the elbow stuck in a bent position at rest. The second scenario is incoordination of muscles due to tone resulting in difficulty with movement. Patients often describe this as moving against quicksand.
Generally treatment of spasticity includes physical and occupational therapy. Several philosophies are used to train muscle to control tone and work toward coordinated movement. Other modalities used include heat and cold, serial casting, biofeedback, relaxation techniques and functional electrical stimu-lation. Maintaining range of motion is key to management of spasticity which requires a consistent stretching program. If the limbs are not stretched daily, the limb can become permanently contracted or “stuck” into a position. This can complicate maintenance of hygiene, limb deformity which can inter-fere with care and recovery , and increased pain. Resting splints and dynamics splints may be used to maintain limbs in a stretched position at night.
Medications can be used to help control spasticity include: baclofen, tizanidine, valium, and/or dantrolene. Other treatments include injections of botulinum toxin into the affected muscle and im-plantable devices such as an intrathecal baclofen pump. In severe cases where spasticity has not been managed, contractures can occur which are fixed positons of the limbs. The only treatment at this stage would be surgical intervention to allow for proper position of the limb to maintain hygiene or proper seating alignment in wheelchairs. Our physicians are experts in management of spasticity and always take into account the patient’s function while caring for the patient.
Amputation and limb deficiencies
 There are two types of amputations: traumatic and nontraumatic. Traumatic amputations occur as an occupational hazard or secondary to major trauma such as a motor vehicle collision or fall. Typically traumatic amputations heal well with minimal complications. Non-traumatic amputations are second-ary to complications of diabetes mellitus, vascular, or infection. These non-traumatic amputations may take a longer time to heal.
There are two types of amputations: traumatic and nontraumatic. Traumatic amputations occur as an occupational hazard or secondary to major trauma such as a motor vehicle collision or fall. Typically traumatic amputations heal well with minimal complications. Non-traumatic amputations are second-ary to complications of diabetes mellitus, vascular, or infection. These non-traumatic amputations may take a longer time to heal.
Following an amputation, patients may experience phantom pain or sensations. Phantom pain is the sensation of pain to the part of the body that is no longer present. Phantom sensation is sensation of the body part moving and can be described as itching or the feeling of movement e.g.(toes are curling). These sensations generally decrease with time. Medications to treat phantom pain may be used early if this is bothersome.
Postoperatively, the limb that is amputated is elevated and wrapped in a simple dressing. It is often recommended that a compression garment is used to help with swelling and pain associated with swelling. Maintaining range of motion in all joints remain is key to preparation for prosthesis management. Following amputation, patients may be discharged to home, inpatient rehab, long term acute care facility, or skilled nursing facility. The goal for patients following lower limb amputations are to be able to transfer to a wheelchair, toilet or bedside commode, dress upper and lower body and perform hygiene from a seated position, navigate a wheelchair household distances (typically 100-150 feet) and walk short distances by hopping on the sound limb with a use of rolling walker.
Prosthetic fitting does not occur until the incision has healed and can range from 4 weeks, typically in a traumatic health individual to 12 weeks in a complicated individual with circulatory deficits. This hap-pens as an outpatient. Prosthetic components vary depending on the individual’s capacity for activity.
Once the preliminary prosthesis is made, a wearing schedule is used to allow the limb to become accustomed to the feel and the pressure placed on the residual limb. Once the preliminary prosthesis is tolerated for at least a period of thirty minutes, therapy can commence and the patient learns to walk using the prosthesis.
Over time, the limb will shrink which is normal. As the patient becomes accustomed to prosthesis, he/she can potentially advance their activities. During this time, the prosthetist will work with the pa-tient to adjust fit and componentry before the definitive prosthesis is made. The definitive prosthesis is made once the residual limb is stable and no little limb change is expected and the right components are selected that is expected to accomplish that individual’s goals. This process can take up to a year. This definitive prosthesis is expected to be able to worn about 5 years with replacement of parts depending o wear and tear. Our physicians are experts in this field and work with patients as early as when they are inpatients all the way until they are outpatients.
HOSPITAL : INPATIENT REHAB, CONSULTS, SKILLED NURSING FACILITY, LONG TERM ACUTE CARE
Our physicians see patients in the office and at various local hospitals. There are various levels of care and our physicians cover all those levels. We see patients in the acute hospitals (Plaza, Baylor All Saints, and Harris Methodist (THR)) and provide consultation when asked by the admitting physician. We see a myriad of diagnosis including strokes, brain injuries, amputees, and patients after orthopedic surgeries to name a few. Our physicians will help initiate the rehab process in the hospital and then discuss with the patient, family, and other physicians our recommended next step involving rehab (do you go home, to a rehab hospital, to a skilled nursing facility, to long term acute care, etc).
Our physicians admit patients to Inpatient Rehab Hospitals as well. These hospital offer 3 hours/day of therapy and the patients care is guided by a Physical Medicine and Rehabilitation physician.
Our physicians also offer consultations at various Long Term Acute Care hospitals (LTACs) and Skilled Nursing Facilities (SNFs or SNUs). At these facilities we will guide the patient’s rehab course by com-municating with the therapy team, case managers, and the physicians involved in that patient’s care.
You can call our office at 817-336-7188 and ask our staff which hospitals, inpatient rehab facilities, long term acute care hospitals, or skilled nursing facilities our physicians are going to as that list may be sub-ject to change from time to time therefore it is not published here.


